LOS ANGELES, Calif. – Sept. 30, 2013 – Twelve generous yet ordinary people who donated a kidney so that others could live have been selected to walk alongside the 11th annual Donate Life float in the 2014 Rose Parade, themed "Light Up the World." The living donors will walk the five-mile parade route to underscore the possibility of donating a life-saving organ while alive as well as demonstrate the vitality of people who have done so.
"As we begin our second decade of Rose Parade participation, we felt it important to honor the generosity of living donors, who are beacons of hope to people suffering from kidney failure," stated Bryan Stewart, chairman of the Donate Life Rose Parade Float Committee and vice president of communications at OneLegacy, the non-profit organ, eye and tissue recovery organization serving the greater Los Angeles area.
Each year, about one-third of the nearly 17,000 kidney transplants nationwide involve living donors. The recipients are mostly family and close friends of the donors, but increasingly often altruistic donors step forward to donate to a stranger, with the potential to start a chain of kidney transplants that can potentially free dozens of kidney patients from dialysis. Because the conditions allowing deceased donation to occur are extremely rare, increasing living donation is essential to helping the nearly 100,000 individuals currently awaiting a kidney transplant. Living donors also account for about four percent of liver transplants.
Five of the walkers will be just steps from their recipients riding on the Donate Life float.Kathleen and Justin Hostert (Fullerton, Calif.) both gave kidneys to float rider Craig Hostert, their husband and father, respectively. Kathleen's donation was 14 years ago; Justin's was last December. The family of four leads a 60-person committee to produce the Donate Life Run/Walk each April at Cal State Fullerton, the nation's largest donation-themed event.
Michael Cervantes (Chino, Calif.) will walk next to his brother and recipient, rider John Cervantes, whose transplant brought an end to 30 years of kidney-related health challenges and allowed him to return to his 17-year career as a police officer.
Lakishia White (Fresno, Calif.) and Jessica Jurado (Sacramento, Calif.) will walk alongside Lakishia's husband, rider JePahl White, who received his second kidney from Jessica via a paired exchange program. Jessica gave her kidney to JePahl, while LaKishia gave her kidney to a recipient in Pennsylvania. In turn, Jessica's mother received a kidney from another participant in the exchange.
Two walkers were inspired to donate by seeing stories about donation.
Phillip Palmer(West Monroe, La.), news anchor at ABC7 Los Angeles, read a story about then-NBA star Sean Elliot, who received a kidney from a living donor. The concept of living donation was entirely new to him, but he knew he wanted to give to someone, some day. Years later, his co-worker and friend Dale Davis sickened quickly from kidney failure, and Phillip stepped up to donate his kidney. He encourages people to talk about donation. "You never know how that conversation will end or the lives you might save," he declared.
Kelly Wright, DVM (Newport Beach, Calif.) was inspired by seeing the Donate Life float in the 2013 Rose Parade. She resolved then to give one of her kidneys to a stranger, and through Facebook met a father of two in Massachusetts who was spending 12 hours a week on dialysis. Three months later, the transplant was a success. "I will never have a bigger accomplishment in my life than having one of my kidneys working inside of another human being who may have died without it," she reflected. "Living donation is a blessing for both donor and recipient."
Karen Willis (Northridge, Calif.) wanted to help a complete stranger in a big way; the idea of donating a kidney came very quickly. She liked the idea of helping many people in a kidney chain with her one altruistic donation. Through her participation in "The Chain," a documentary about the series of transplants she initiated, Karen was able to meet two other donors and two recipients, including her own. "I gave three people back their health, their dreams, and their ability to have a quality life with their families," Karen said.
Another who gave to a stranger was Teresa "Terie" Cota (Santa Maria, Calif.), who wanted to help someone else when she was not able to help her brother-in-law, Chris, who succumbed before the transplant could occur. Teri believed that her kidney could still help someone else through a non-directed donation. On the one-year anniversary of Chris's death, Terie received the news that a recipient had been found. "The decision was simple," she said. "I had been given the gift of health, and I wanted to share it. I believe the opportunities to make choices like these are the best part of being human."
Through his longtime career in tissue banking, Kevin Lucien Noyes (North Branch, Minn.) has long understood the importance of and need for organ and tissue donation. In March 2011, he learned that Marlin, his high school math teacher and father of a lifelong friend, needed a kidney transplant. Drawing on his conviction to do the right thing, Kevin underwent testing, lost weight to meet the transplant center's requirements, and restored life for Marlin. Kevin hopes his story inspires others to explore the opportunity for themselves.
Kathy Vochoska (Bakersfield, CA) watched as her college son Chris went into sudden kidney failure due to Berger's Disease. With Chris on dialysis, the need for a kidney was imminent, especially from a living donor in the family. Kathy found she could be his match, and she donated her kidney to him at the end of March 2011, and subsequently became a Donate Life Ambassador. "Although I hate that my son got sick, the silver lining of our journey is that I am now involved with the most compassionate and inspiring group of people I have ever met," she said. "My life has been forever changed."
J
eff E. Carter, Jr. (Getzville, NY) also had a son, Jeff III ("Jeffrey"), who developed kidney disease. Four years after being diagnosed with kidney disease, 18-year-old Jeffrey's kidneys completely shut down, followed by three years of dialysis and numerous hospitalizations, surgeries, and near-death occasions. Once Jeffrey was cleared for a kidney transplant, Jeff did not hesitate to donate. Tragically, however, nine years after he donated his kidney, Jeff's youngest daughter Rebekah died. "Rebekah's organs and tissues were donated, and we know that her life continues in others," said Jeff.
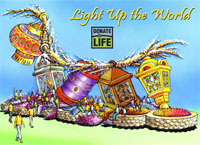
The 2014 Donate Life Rose Parade Float entry features a festival of lanterns illuminating 30 riders and 12 living organ donors walking alongside the entire five-mile route. The float's five enormous lanterns are adorned with 78 memorial floragraph portraits of deceased donors whose legacies of life shine brightly. The riders are seated throughout a dedication garden filled with thousands of roses bearing personal messages of love, hope and remembrance.
Since its debut on New Year's Day 2004, the Donate Life Rose Parade float has become the world's most visible campaign to inspire people to become organ, eye, and tissue donors. The campaign began as an idea expressed in a letter by lung recipient Gary Foxen of Orange, Calif., who wanted to show gratitude to donors who make life-saving transplants possible. Now, in addition to the 40 million viewers who view theRose Parade in the stands and on TV, hundreds of events are held in cities and towns around the country to put the finishing touches on floragraph portraits and present dedicated roses to donor families and community partners that play a role in making donation possible.
The 2014 Donate Life float is built by Phoenix Decorating Company from a design by Dave Pittman and is coordinated by Los Angeles-based OneLegacy, the world's largest organ, eye and tissue recovery organization. Each year, the Donate Life float campaign is supported by more than 140 official sponsors from coast to coast, including organ, eye and tissue recovery organizations, tissue processors, hospitals, transplant centers, state donor registries, funeral homes, donor family foundations and affiliated organizations.
Joining OneLegacy as top-level benefactors are:
American Association of Tissue Banks (AATB), which is dedicated to ensuring that human tissues intended for transplantation are safe and free of infectious disease, of uniform high quality, and available in quantities sufficient to meet national needs;
Dignity Memorial® network, North America's largest network of funeral, cremation and cemetery service providers;
Donate Life America, a nonprofit alliance of national organizations and state teams across the United States committed to increasing organ, eye and tissue donation;
Donate Life Run/Walk Committee, the Orange County-based producer of the nation's largest donation-themed 5K fundraising event;
Josiah's House, a Tennessee-based nonprofit ministering to boys in the Dominican Republic in honor of Josiah Berger;
The Order of St. Lazarus, an international community of Christian men and women devoted to ecumenical spirituality, worldwide charity and chivalric tradition;
SightLife, a nonprofit eye bank focused on eliminating corneal blindness in the United States and worldwide; and
TBI/Tissue Banks International, a nonprofit network of eye and tissue banks and the largest provider of ocular tissue in the world.
The Donate Life Rose Parade Float's family of sponsors urges viewers to help make dreams come true for more than one million people in need of life-saving and healing organ, tissue and cornea transplants. Join America's 113 million registered donors so that everyone whose life and livelihood depends on a transplant can have one. Sign up when renewing your driver's license or by visitingwww.DonateLifeAmerica.org. Further information about the Donate Life float can be found at www.donatelifefloat.org.
The Pasadena Tournament of Roses is a volunteer organization that annually hosts the Rose Parade® presented by Honda, Rose Bowl Game® presented by VIZIO and various associated events. The 125th Rose Parade presented by Honda, themed "Dreams Come True," will take place Wednesday, Jan. 1, 2014, at 8 a.m. (PST) featuring majestic floral floats, high-stepping equestrian units and spirited marching bands. Following the parade, the 100th Rose Bowl Game presented by VIZIO will kick off at2:10 p.m. and feature an exciting match-up between two of the top collegiate football teams in the nation. For additional information on the Tournament of Roses please visit the official website at www.tournamentofroses.com.
“You Have the Power to Donate Life – Sign-up today! Tell Your Loved Ones of Your Decision”